Pathogenic bacteria
Detect pathogens that can cause food poisoning
- Home
- /
- Analytes
- /
- Microbiology
- /
- Pathogenic bacteria
Pathogenic bacteria in food production: Risks, detection, and prevention
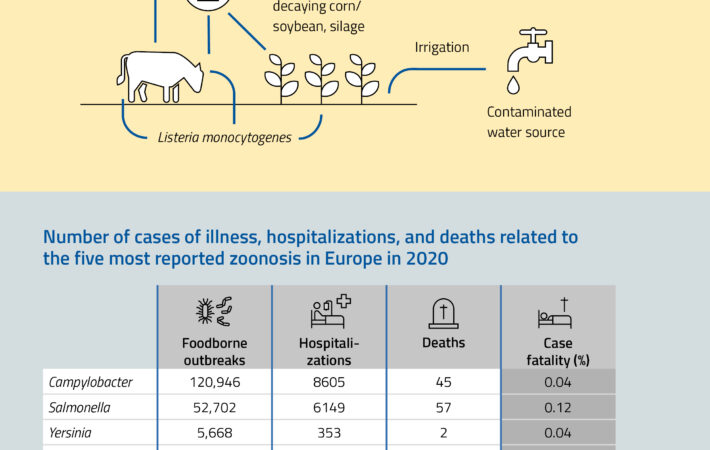
Understanding pathogenic bacteria in food safety
Pathogenic bacteria are harmful microorganisms that can contaminate food and cause serious illnesses in humans. These bacteria, including Salmonella, Listeria monocytogenes, Escherichia coli (E. coli), and Campylobacter, thrive in various food products and environments. Ensuring that food is free from dangerous bacteria is crucial for public health, as foodborne illnesses can lead to severe complications, hospitalizations, and even fatalities.
Sources and risks of pathogenic bacteria contamination
Food contamination can occur at multiple stages of the production chain, from raw materials to finished products. Some of the most common sources of pathogenic bacteria include:
- Raw meat and poultry – Can harbor Salmonella, E. coli, and Campylobacter if not handled or cooked properly.
- Dairy products – Unpasteurized milk and soft cheeses can contain Listeria and E. coli.
- Fresh produce – Fruits and vegetables can become contaminated through irrigation water or improper handling.
- Seafood – Shellfish and fish can carry Vibrio bacteria if sourced from contaminated waters.
- Processed and ready-to-eat foods – Cross-contamination during manufacturing or storage can introduce bacteria.
Given the widespread risks, stringent food safety measures are necessary to prevent bacterial growth and contamination.
Together with Salmonella, Campylobacteriosis is one of the most significant diarrheal diseases worldwide. The increase in Campylobacter enteritis is driven by the widespread presence of the bacterium in various wild and farm animals, as well as pets. As a commensal in the gut of poultry, Campylobacter enters the human food chain via these animals. Additionally, milk, ground meat, and drinking water can act as transmission pathways. Campylobacter is released in high quantities by numerous hosts, contaminating food and reaching humans. The infective dose for Campylobacter enteritis is low, requiring fewer than 500 bacteria to cause infection. Of the approximately 15 known Campylobacter species, C. jejuni and C. coli are the primary causes of human gastroenteritis.
Clostridium species are gram-positive, spore-forming bacteria present almost everywhere in the environment. Important pathogenic species include Clostridium botulinum, Clostridium perfringens, and Clostridium estertheticum. If food is not adequately cooled, it can become contaminated, leading to serious illnesses. These bacteria are heat-resistant and can survive in thoroughly heated food products.
Legionella are gram-negative, rod-shaped bacteria that live in water and are considered potential human pathogens. Legionella pneumophila is the species most responsible for human illnesses, causing Legionnaire’s disease (legionellosis). The disease is typically transmitted through contaminated drinking water.
Listeria bacteria are ubiquitous in the environment. Quantitative detection of Listeria can assess contamination risk and ensure preventive measures are taken if necessary. Listeria monocytogenes is a major cause of food poisoning and can lead to sepsis, meningitis, and encephalitis.
Salmonella is ranked among the most important initiators of cases of food poisoning. The WHO estimates more than 16 million global infections per year, and more than half a million cases are fatal. Salmonella are found in raw food such as eggs, meat and milk. The hazard potential is high, particularly in food that should only be slightly heated or not at all heated (e.g. raw milk cheese, raw sausage, chocolate, ice cream). In today’s mass animal farming industry, contaminations with Salmonella can hardly be avoided. Therefore, effective quality control with reliable test methods is important. For this purpose, we offer a series of different test systems, for the hygienic control of surfaces as well as for the analysis of food.
Staphylococcus aureus is a ball-shaped bacterium which can be observed as a grape-like clustered organism under the microscope. Cells are sized between 0.8 and 1.2 µm, Gram-positive and non-motile. S. aureus is a natural commensal of humans which lives on skin and upper airways and doesn’t cause diseases in general. In case of infections with pathogenic strains or in immunodeficient persons, S. aureus is able to cause skin infections and abscesses but also life-threatening diseases as pneumonia, meningitis, endocarditis, or toxic shock syndrome (TSS).
One reason for the facultative pathogenicity of S. aureus is its ability to form enterotoxins (SET), which can accumulate in contaminated food and cannot be inactivated totally by heat treatment. Contamination of foodstuffs with S. aureus is almost always caused by humans (hands, sneezing, coughing). S. aureus is therefore considered as indicator for poor personal hygiene.
Beside its relevance for food hygiene, S. aureus also plays a significant role in hospital hygiene. Especially strains of S. aureus which have acquired resistances against common antibiotics the so-called „methicillin resistant Staphylococcus aureus” (MRSA) might pose a non-assessable danger as they are difficult-to-treat.
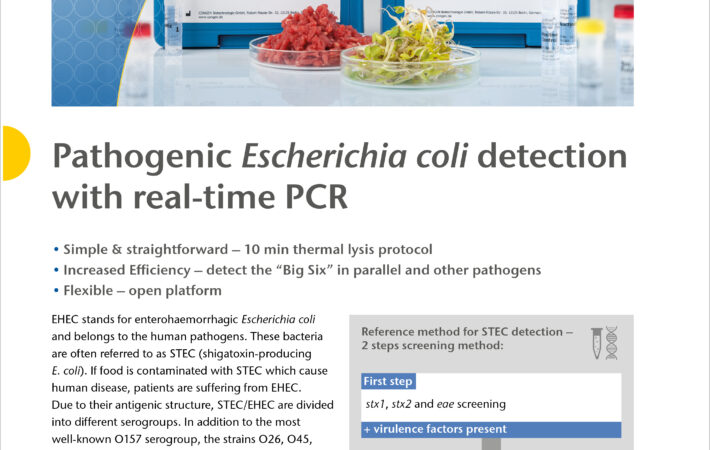
The bacteria Escherichia coli (abbreviated E. coli) is a natural component of the intestinal flora in humans and animals and it is usually harmless. However, there are pathogenic strains that can cause serious infections. One of these pathogenic strains is known as enterohemorrhagic Escherichia E. coli (“EHEC”). These bacteria build the toxic substances verotoxin or shiga toxin and are also known as verotoxin-producing E. coli (“VTEC”) or shiga toxin-producing E. coli (“STEC”). Infections with STEC/VTEC are ranked as one of the most common food-related bacterial diseases that can even result in death. Sources of contamination mainly include raw meat and unpasteurized dairy products.
The group of Vibrio spp. includes pathogenic microorganisms which can cause serious infections after consumption of contaminated food. In diseases correlated to seafood, Vibrio spp. is one of the major causes of gastroenteritis, wound infection and sepsis. Additionally, in serious infections with the potential for epidemics such as Cholera, Vibrio spp. is causative.
The bacterium Vibrio parahaemolyticus naturally inhabits coastal waters and is present in higher concentrations during summer. The organism is halophilic or salt-requiring. Therefore, Vibrio parahaemolyticus is found in marine environments, seafood and the feces of patients with acute enteritis. Vibrio parahaemolyticus-associated gastroenteritis is the infection caused by this organism.
Importance of detecting and controlling pathogenic bacteria
To protect consumers and meet regulatory requirements, food manufacturers and quality assurance teams must proactively detect and control pathogenic bacteria in their production processes. Implementing advanced bacterial detection methods ensures food safety and helps prevent outbreaks. Contamination in food products can lead to costly recalls, legal issues, and reputational damage for brands.
Advanced testing solutions for pathogenic bacteria detection
R-Biopharm offers highly sensitive and specific test systems designed for the rapid and reliable detection of pathogenic bacteria in food production environments. These testing solutions provide critical advantages for food manufacturers and regulatory bodies:
- Rapid and reliable results – Fast detection of Listeria, Salmonella, E. coli, and other pathogens to prevent foodborne illnesses.
- Comprehensive monitoring – Tests for raw materials, finished products, food contact surfaces, and production environments.
- Easy integration into HACCP systems – Ensures food safety compliance with minimal workflow disruption.
- High sensitivity and specificity – Detects low bacterial levels to prevent contamination before products reach consumers.
- Regulatory compliance – Supports adherence to international food safety standards, including HACCP, ISO 17025, and FDA/EFSA guidelines.
Best practices for preventing pathogenic bacteria contamination
In addition to using advanced detection systems, food producers must adopt best practices to minimize contamination risks:
- Strict hygiene protocols – Regular handwashing, sanitization of equipment, and proper food handling procedures.
- Temperature control – Proper refrigeration and cooking temperatures to inhibit bacterial growth.
- Cross-contamination prevention – Separation of raw and cooked foods, proper storage, and dedicated food preparation areas.
- Water and environmental monitoring – Regular testing of processing water and facility surfaces for bacterial presence.
- Employee training and compliance – Continuous education on food safety protocols and hazard prevention.
Ensuring food Safety with R-Biopharm’s test systems
Foodborne pathogens pose significant health risks, making reliable detection and prevention strategies essential for the food industry. R-Biopharm’s test systems offer a robust solution to identify, quantify, and control pathogenic bacteria at every stage of food production. By integrating these tests into a comprehensive HACCP plan, food manufacturers can enhance consumer safety, maintain regulatory compliance, and protect their brand reputation.
For more information on our advanced bacterial detection solutions, contact R-Biopharm today and safeguard your food production against pathogenic bacteria.